Overview: From Episodic Care to a Screening Operating System
Saudi Arabia’s new “Taakkad” preventive screening initiative marks a structural turn in how the Kingdom plans to manage chronic disease risk.
In January 2026, the Health Holding Company (HHC) and Ministry of Health (MOH) announced the operational rollout of Taakkad: a national program that lets adults 35+ book standardized screening packages digitally via Sehhaty, attend drive through clinics across Riyadh’s health clusters, and receive integrated follow up in the public system.
Underneath the press language, Taakkad is doing three system level things that matter to investors and policy observers:
- Standardizing preventive pathways (from ad hoc tests to designed packages).
- Digitizing access and logistics (Sehhaty booking, drive through workflows).
- Creating a longitudinal data spine that ties screening, risk scoring, and follow up care into one loop.
That positions Taakkad less as a “campaign” and more as infrastructure: a risk detection layer on top of Saudi’s NCD burden, into which workforce, insurers, digital health companies, and med tech suppliers will plug over the coming decade.
For investors, the question is not whether preventive screening is “good public health” that’s settled. The question is: how does a structured, state scale program like Taakkad change utilization curves, cost trajectories, and private sector revenue opportunities?
This article unpacks that question across the global, regional, and Saudi context, then links Taakkad to concrete investment and partnership theses.
Global Landscape: NCDs, Prevention and the Economics of Early Action
Non communicable diseases (NCDs) cardiovascular disease, cancer, chronic respiratory disease, and diabetes are now the dominant source of mortality worldwide. Updated WHO fact sheets estimate that NCDs caused at least 43 million deaths in 2021, roughly 75% of non pandemic related deaths, with around 18 million deaths before age 70.
Two global trends are relevant for Taakkad:
Shift From Treatment to Prevention
NCD policy has moved from hospital centric care to population level prevention “bundles”: tobacco taxes, salt and sugar reduction, physical activity promotion, and organized screening programs for cancers and cardiometabolic risk. Global guidance increasingly frames screening not as a one off test, but as a designed pathway: outreach, test, risk stratificationm structured follow up.
Growing Evidence for Macro Economic Returns
Economic evaluations for multiple regions now show that high impact NCD interventions especially hypertension and diabetes control and cancer screening deliver net positive returns when modelled to 2030, with benefit cost ratios above 1 in most scenarios.
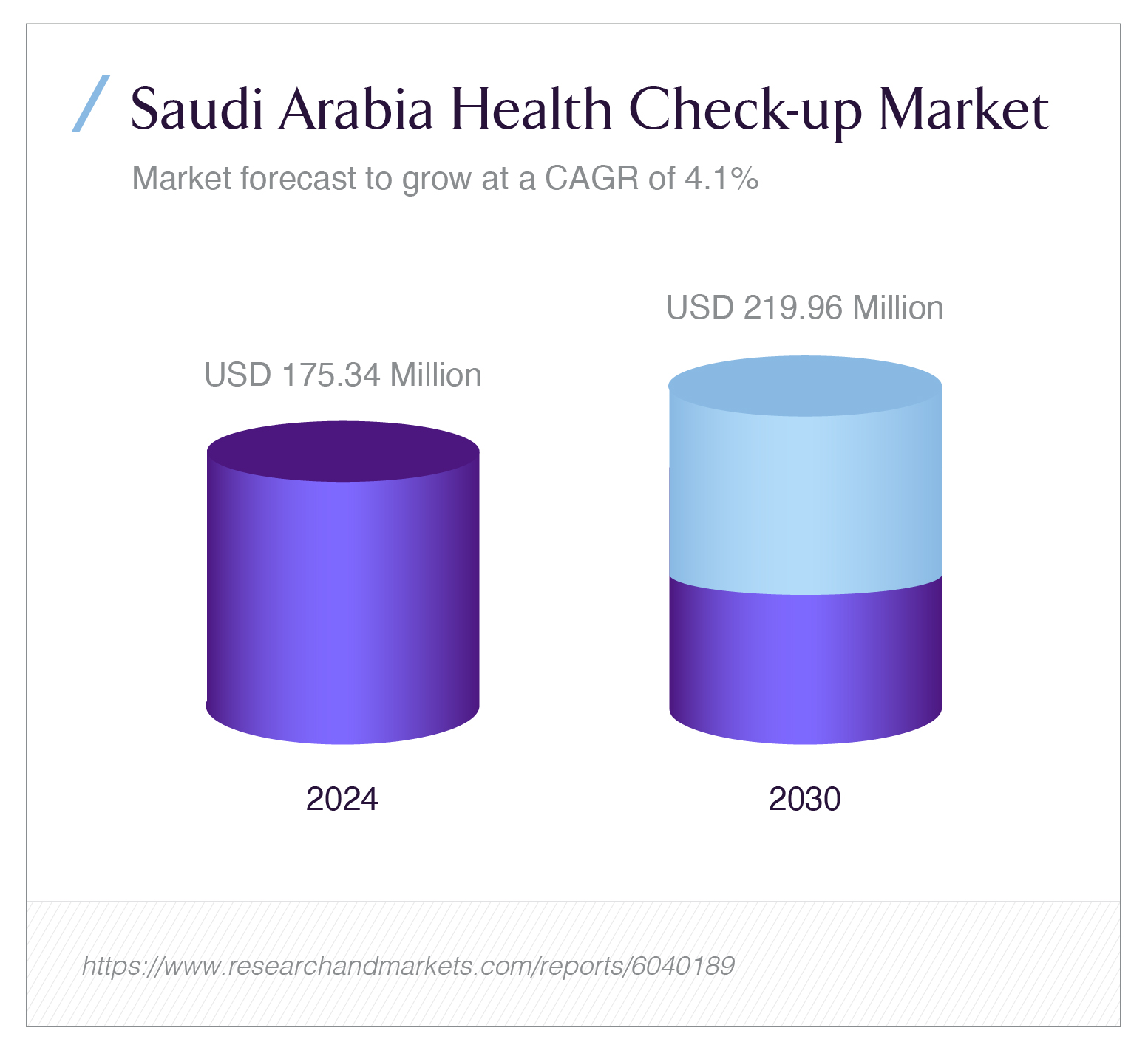
The global market has responded. Commercially, preventive health check up and screening markets have become stand alone verticals. For example, Saudi Arabia’s own health check up market (not yet counting Taakkad) was valued at USD 175.34 million in 2024 and is expected to reach USD 219.96 million by 2030, a CAGR of about 4.05%.
Globally, that growth is underpinned by a simple ratio: 1 unit of spending on structured prevention and early detection can avert multiple units of hospital based cost and lost productivity later, particularly where hypertension, diabetes and cancer remain under diagnosed until late stages.
Taakkad is Saudi Arabia’s attempt to internalize that ratio into the public system, using state infrastructure and data to make preventative screening a default behaviour, not an exception.
Regional Landscape: GCC’s NCD Costs and the Case for Structured Screening
Across the GCC, NCDs have become a material macro economic risk. A synthesis of GCC NCD investment cases estimates that the four main NCDs (cardiovascular disease, diabetes, cancer and chronic respiratory diseases) now cost GCC economies around US$50 billion annually, roughly 3.3% of regional GDP, with about 60% of that cost coming from direct treatment.
The Gulf’s health system response so far has had three characteristics:
- Significant capital into tertiary care large hospitals, specialized centres, and advanced therapeutics.
- Fragmented preventive efforts campaigns, workplace programs, and ad hoc screening days, often disconnected from long term follow up.
- Patchy data on screening coverage and outcomes, making it difficult to quantify the ROI of prevention at system scale.
Saudi’s Public Health Authority (PHA) and MOH have been moving to close those gaps. The NCDs Prevention and Control Plan (2024-2030), published by PHA, explicitly calls for increased screening coverage for hypertension, diabetes, obesity, and major cancers, and lays out a multi sectoral implementation framework with quantified investment needs and health outcomes.
Crucially, that plan models the costs and returns of high impact interventions over 2024-2030.

The chart shows a front loaded investment profile with spending ramping up in early years but more importantly, it sits alongside a second chart that captures the payoff.
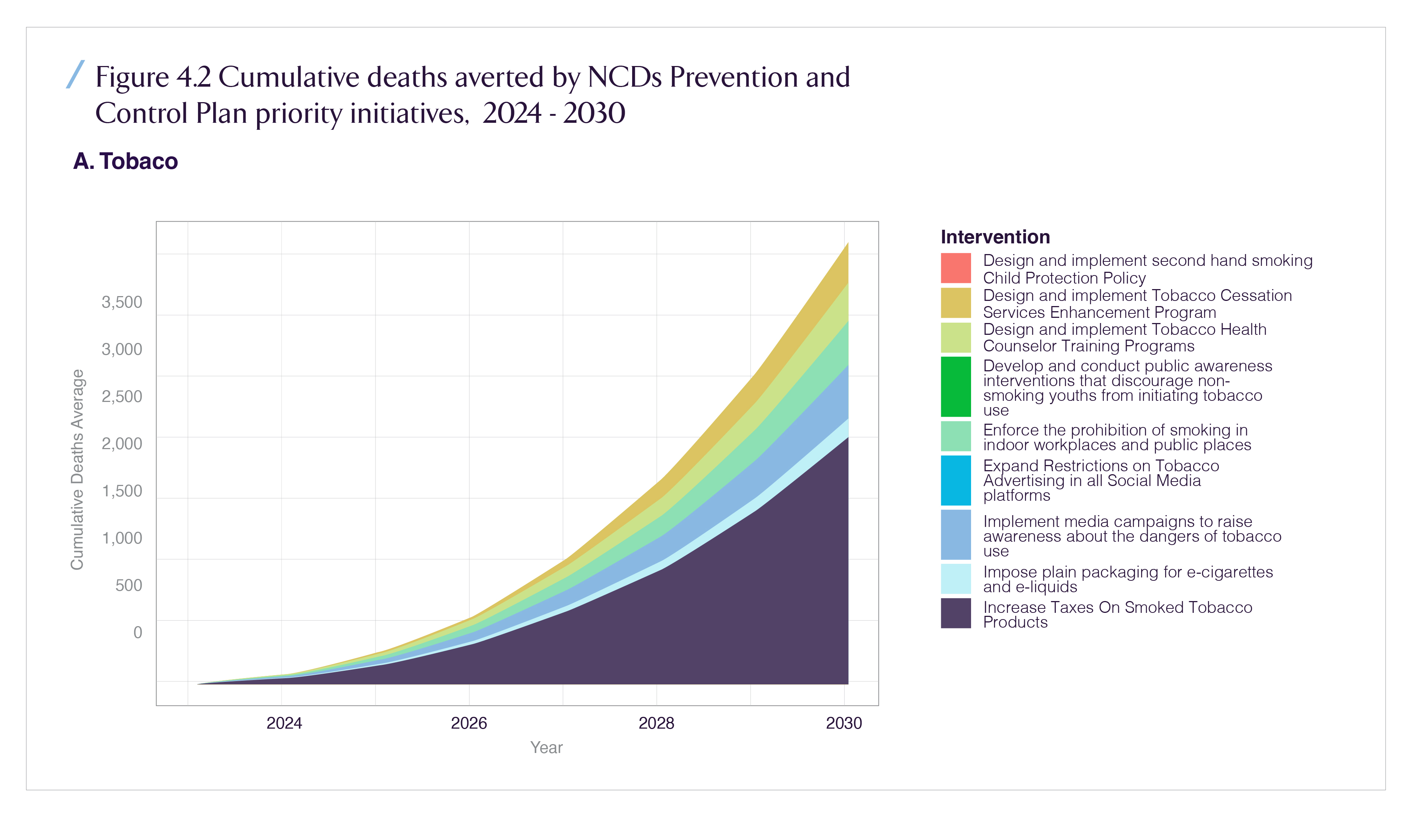
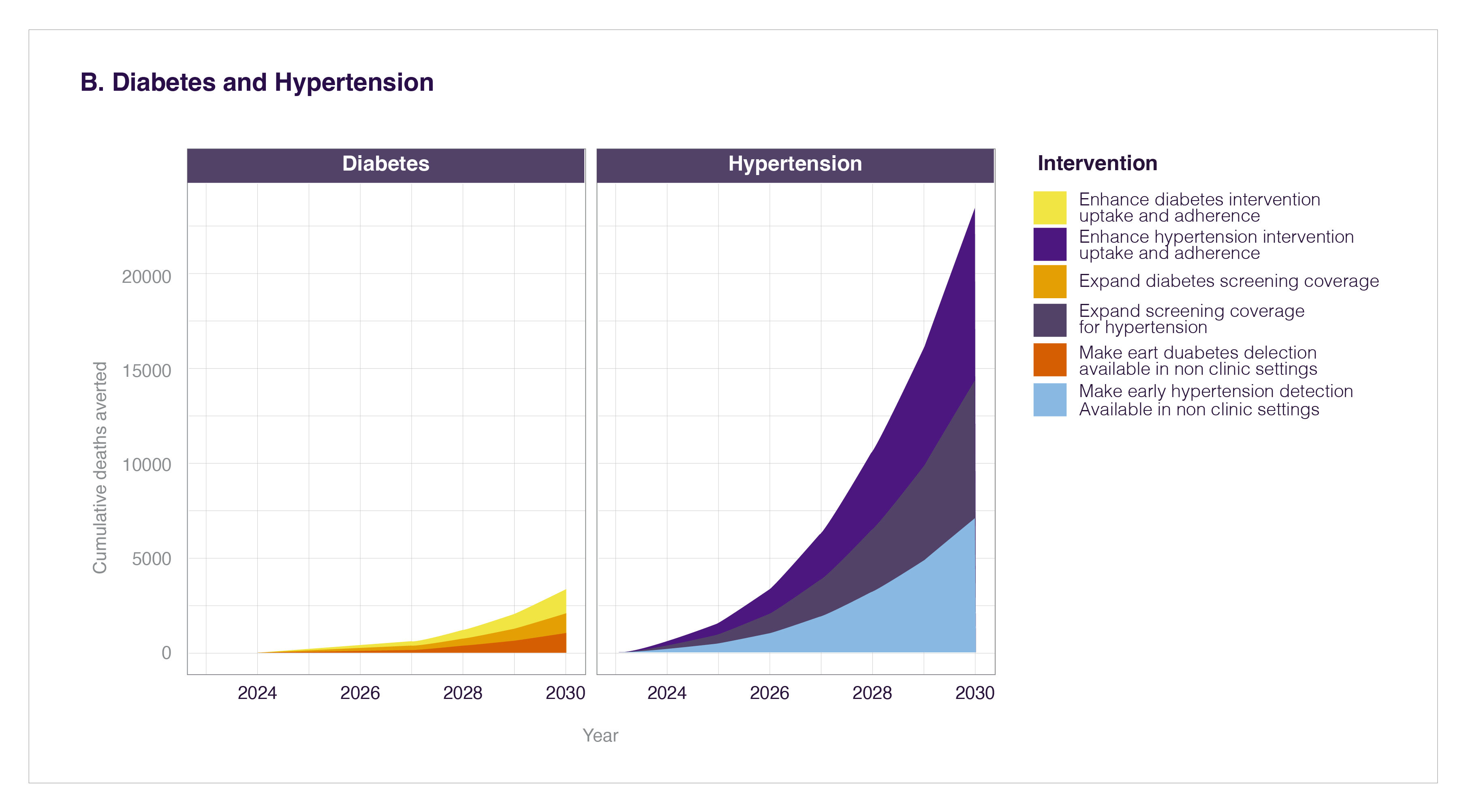
Taakkad becomes the on the ground execution layer for those modelling assumptions: it is how the system converts investment in prevention into actual tests, diagnoses, and behaviour change.
Saudi Landscape: Taakkad as the Practical Face of the NCD Plan
How Taakkad Actually Works
The January 6, 2026 MOH announcement describes Taakkad as a national preventive program, initially active in Riyadh’s health clusters, where adults 35 years and older can book appointments through Sehhaty by selecting a dedicated “Taakkad Clinic Adult Triage” option. Clinics are configured as drive through service pathways to minimize friction and throughput constraints.
Taakkad currently offers three structured screening packages:
- Basic Package screens for diabetes, lipid disorders, high blood pressure, BMI and related metabolic risk.
- Basic Plus Package adds advanced tests for early detection of selected cancers (including breast and colorectal) and bone health conditions such as osteoporosis.
- Advanced Package (announced) will introduce genomics, proteomics, and lifestyle analysis based risk prediction.
These packages mirror the priority conditions highlighted in PHA’s NCD strategy (hypertension, diabetes, cancer, obesity, tobacco use), but translate them into practical bundles a citizen can understand and complete in a single visit.
Interaction With the Broader Screening Market
From a market structure perspective, Taakkad lands in a landscape where preventive health check ups are already a growing commercial vertical:
- TechSci / ResearchAndMarkets estimate the Saudi Arabia health check up market at USD 175.34 million in 2024, rising to USD 219.96 million by 2030, implying steady expansion of private offers in corporate and retail segments.
- Ken Research, in an October 2025 note, values the broader preventive healthcare screening market (which includes imaging, lab diagnostics and wellness packages) at about USD 1.2 billion, with growth driven by rising chronic disease incidence, government initiatives, and technology adoption.
Taakkad does not replace this private capacity. Instead, it:
- anchors baseline access to essential screening in the public system,
- creates standardized benchmarks for what a “complete” preventive package looks like,
- and generates population scale risk data that can inform both public planning and private product design.
For investors, the key is to see Taakkad as a public spine around which private offerings will differentiate (depth of tests, value added coaching, employer tailored programs) while referencing common guidelines.
Challenges: Where the System Must Still Execute
Taakkad’s design addresses several long standing gaps but it also surfaces execution risks that matter for capital allocation and partnership strategies.
1. Coverage and Uptake
Screening only works if people show up before symptoms. Historically in Saudi Arabia, uptake of opportunistic screening for hypertension, diabetes and certain cancers has lagged behind desired levels, especially among lower income and rural populations. PHA’s own analysis highlights under diagnosis and late presentation as major drivers of NCD burden.
Taakkad’s drive through model and digital booking reduce friction, but uptake will still depend on:
- awareness campaigns targeted by age, gender, and risk profile;
- integration with workplace policies (e.g., paid time off for screening days);
- culturally sensitive communication around cancers and metabolic disease.
2. Integration With Care Pathways
Screening without structured follow up risks generating “ghost positives”—abnormal findings that never convert into treatment or lifestyle change.
The success of Taakkad will hinge on:
- how seamlessly results flow into primary care clinics and virtual consults,
- whether risk stratified recall (e.g., 3, 6, 12 month follow up) is automated,
- and how co morbidities (e.g., diabetes + obesity + hypertension) are managed across silos.
From an IT and workflow perspective, this demands robust interoperability between Sehhaty, HHC cluster systems, and national registries.
3. Data Quality, Analytics and Governance
Taakkad will generate a new stream of longitudinal biometric, lab, and lifestyle data. Turning that into value requires:
- consistent coding and data standards;
- rules on data use for planning vs. research vs. commercial partnerships;
- analytics capacity to translate raw screening data into risk maps, cohort trajectories, and intervention targeting.
For investors, this is where data platforms, AI driven risk engines, and privacy preserving analytics will likely emerge as opportunity zones but only if governance frameworks are clear.
4. Workforce and Capacity
Scaling Taakkad from Riyadh to national coverage will stress workforce and logistics. Even with automation, the program needs:
- lab capacity (for high throughput processing of tests),
- trained nurses and technicians for drive through clinics,
- and sufficient specialist back up (e.g., endocrinology, oncology, cardiology) for positive cases.
The key risk is capacity bottlenecks that delay confirmatory diagnostics or treatment, eroding the value of early detection.
Solutions and System Levers: How Taakkad Can Be Engineered for Impact
From an investor and policy design perspective, Taakkad is not just a set of clinics; it is a platform that can be tuned.
1. Risk Stratified Population Design
Using NCD risk factors and Taakkad data, HHC can segment the adult population into risk tiers (e.g., low, elevated, high, very high) and tailor:
- screening frequency,
- test depth (basic vs. advanced packages),
- and behavioural support intensity (digital coaching, SMS nudges, workplace interventions).
Linking this to PHA’s investment models where specific combinations of interventions have quantified deaths averted turns Taakkad into a live implementation of the NCD investment case.
This is where the chart stops being abstract. A properly instrumented Taakkad can:
- track how much of the modelled mortality reduction is being realized,
- identify geographic or demographic pockets where uptake is low,
- and re allocate outreach or add mobile units to close gaps.
2. Embedding Taakkad Into Employer, Insurer and PHC Contracts
For the private sector, Taakkad is a natural anchor for contractual metrics:
- Employers can tie wellness benefits and paid screening leave to Taakkad completion rates.
- Insurers can integrate Taakkad adherence into premium differentiation models, especially for group products.
- Primary care providers can be reimbursed or performance rated based on post Taakkad follow up quality (e.g., proportion of newly diagnosed hypertension cases controlled within 6 12 months).
Over time, this moves Taakkad from a “nice public service” to a shared KPI across the ecosystem.
3. Leveraging Technology and AI
Taakkad’s advanced package with genomics, proteomics and lifestyle analytics is a signal that Saudi intends to experiment with precision prevention at scale.
Potential technology levers include:
- AI assisted triage: algorithms that prioritize patients for deeper diagnostics based on combined Taakkad and EHR data.
- Digital twins and risk simulations: projecting individual and cohort trajectories under different intervention mixes.
- Population dashboards: real time visualizations of risk profiles by cluster, age, gender and socioeconomic status.
This is where multiple vendor categories enter: cloud providers, data platform companies, AI as a service firms, and local health IT integrators.
4. Geographic Scaling and Equity
Taakkad’s initial focus on Riyadh clusters is logical from an operational standpoint, but the NCD burden is national.
Scaling Taakkad can follow a phased pattern:
- Phase 1: Riyadh health clusters (current).
- Phase 2: Extension to other major urban regions (Jeddah, Dammam/Khobar) with adaptation to local capacity.
- Phase 3: Expansion to peripheral and rural areas, potentially via mobile and semi mobile Taakkad units, integrated with PHC centers.
Investors eyeing diagnostics, mobile clinic solutions, and digital infrastructure should think in terms of “hub and spoke Taakkad models” rather than static clinic footprints.
Benefits: Why Taakkad Matters for Investors, Not Just Clinicians
1. Macro and Fiscal
At macro level, effective preventive screening helps flatten the curve of NCD treatment cost and extend healthy working life, reinforcing Saudi’s Vision 2030 human capital goals. PHA’s modelling suggests that implementing high impact NCD interventions, of which screening is a core component, can avert a substantial share of projected NCD deaths and reduce long term health system costs relative to a “no additional action” scenario.
For fiscal planners, Taakkad becomes a way to convert upfront operating expenditure into long term fiscal savings and productivity gains precisely the logic that underpins global arguments for investing in prevention.
2. Payers and Employers
For insurers and employers, Taakkad creates:
- Cleaner actuarial data on risk distribution in insured populations.
- Opportunities for shared savings contracts tied to reduced hospitalization and complication rates.
- A foundation for benefit design innovation, such as dynamic co payments or contribution rates linked to screening adherence.
In short, Taakkad can shift the system from paying for episodes to paying for controlled risk.
3. Providers and Med Tech
Providers benefit from earlier case capture (e.g., pre diabetes rather than advanced nephropathy), which changes the mix of services delivered:
- more outpatient and virtual visits,
- more chronic care program enrolments,
- more use of diagnostics and monitoring devices, fewer catastrophic events.
Med tech manufacturers, lab chains, imaging providers, and digital health companies see a more predictable baseline of screening volume, de risking capital investment in capacity and technology upgrades.
4. Data and Analytics Firms
Finally, Taakkad creates an unprecedented data asset. Subject to governance and privacy rules, this opens space for:
- analytics services that help MOH and HHC optimize program design;
- AI powered decision support tools embedded into primary care and hospital EHRs;
- and collaborations on population health dashboards for policymakers and major employers.
For investors, this is not just a health story; it is an infrastructure and data story with direct linkages to cloud, AI, cybersecurity, and analytics portfolios.
Recap: Taakkad as an Investable Public Health Platform
Taakkad is Saudi Arabia’s population scale bet on prevention: a structured, digitally enabled screening program that converts NCD investment cases from PowerPoint into patient flows.
Globally, it sits on top of a clear evidence base: NCDs now cause around three quarters of non pandemic deaths, and prevention focused packages are among the highest ROI public health investments.
Regionally, it responds to a GCC wide NCD bill measured in tens of billions of dollars and several percentage points of GDP.
Nationally, it operationalizes Saudi’s NCD Prevention and Control Plan (2024 2030) and aligns with Vision 2030’s human capital and fiscal sustainability aims.
For investors and strategics, the opportunity is to map their own adjacencies to Taakkad’s architecture:
- diagnostics and lab capacity;
- digital infrastructure and interoperability;
- AI driven risk engines and decision support;
- employer and insurer product design;
- and last mile delivery models for reaching underserved populations.
If Taakkad delivers on its potential, it will not just reduce hospital admissions; it will reset the baseline expectation of what public health looks like in a high income, Vision driven economy and set a benchmark for preventive care platforms across the region.

















